Thousands of children are treated in emergency departments each year after ingesting either button batteries or lithium coin batteries. Both types of batteries are small, shiny and appealing to children. And both can cause major injury if stuck in a child's nose or ear, and possibly even death if swallowed. (See "A Nosebleed," below.)
What are button batteries & lithium coin batteries?
Button batteries and lithium coin batteries are not exactly the same, but both are small round batteries that power many electronic devices. They're found in remote controls and
many other household items. Products designed for children may also contain button batteries or lithium coin batteries, such as some games and toys, and flashing shoes, clothing and jewelry.
How can these batteries injure children?
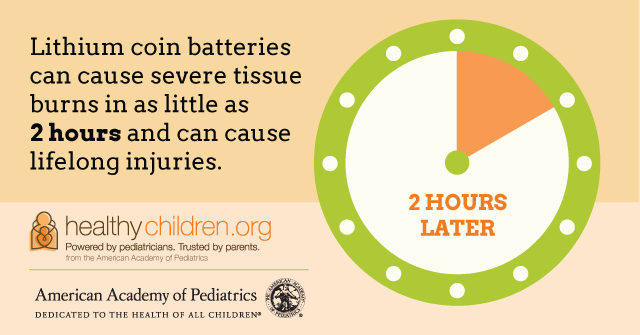
When it comes into contact with body fluids, the battery generates a current. That current produces small amounts of sodium hydroxide, a harsh corrosive similar to lye. If the battery gets stuck somewhere in the body, the lye burns a hole at that spot. Infection usually follows. The result can be serious injury and illness, long-term disability or even death.
What should parents do?
Parents and caregivers should not assume that every battery-powered product that enters their home is safe for use by children. In many products, for example, the battery is easily accessible or can fall out when the product is dropped. Make sure that the battery compartments of all electronic items are secure and taped shut.
When replacing a button battery or lithium coin battery, keep in mind that it stops powering a device way before it runs out of a charge. So, what we think of as a "dead" battery still has the charge to harm a child should it get caught in their
ear, nose, and throat or swallowing passage. The higher the voltage of the battery (3V vs. 1.5V), the faster the injury. To safely dispose of button batteries and lithium coin batteries, wrap them in tape and promptly
recycle or put them in an outside garbage can.
Symptoms
When a child ingests a button battery or lithium coin battery, symptoms could be virtually absent or similar to those of a common infection. This can make it challenging for health care professionals who are evaluating the child.
|
|
When a button battery or lithium coin battery is placed in the nose or ear, there may be noticeable drainage or pain. Since these symptoms are not unique to button battery injuries, and caregivers may not see the child get ahold of the battery, there can be delayed diagnosis and even greater injury. Batteries lodged in the nose or ear can cause extensive damage to structures such as the eardrum and nasal septum. The lye burns can lead to infections and, in some cases, permanent breathing, smell and hearing disability.
When lodged in the esophagus, the lye produced by the electric current rapidly produces burns at that site. The esophagus and nearby structures in the chest can be damaged, including the windpipe, lungs and large blood vessels. Serious infections usually follow, and bleeding caused by blood vessel damage can create an immediate, life-threatening emergency. Survivors may have lifelong disability.
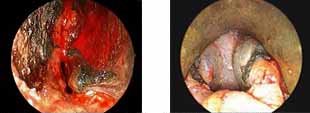 Figure 1
(left): Figure 1 (left): Endoscopic view of button battery injury to nasal septum in right nasal cavity of a child.
Figure 1
(left): Figure 1 (left): Endoscopic view of button battery injury to nasal septum in right nasal cavity of a child.
Figure 2
(right): Rigid esophagoscopy showing button battery injury extending into the muscular layer of esophagus in a child.
Diagnosis & treatment
Once an
x-ray confirms that a button battery is stuck within the body, treatment is urgent removal. The goal is to limit damage to surrounding tissue, and to treat injury that has occurred. A child who has ingested a button battery or lithium coin battery also needs follow-up care to identify long-term and delayed complications.
Awareness is key to prevention
Parents and caregivers need to be aware of the risk posed by button batteries and lithium coin batteries in their home. Keep loose and spare batteries locked away, store any product that uses button batteries or lithium coin batteries out of reach of curious children, and know what to do if they do manage to ingest one. Talk with you pediatrician if you have any questions about your child's safety.
More information