By: Eliza Gordon-Lipkin, MD, FAAP & Paul Lipkin, MD, FAAP
Spina bifida, which affects the spine and spinal cord, is one of the most common birth defects in babies. In fact, it is the most common birth defect of the nervous system. About
1,400 babies are born with the condition in the United States each year.
What is spina bifida?
Spina bifida, which means "split spine," is a
congenital abnormality that occurs before birth. It happens when the embryo's neural tube--which later becomes the brain and spinal cord—does not close all the way. This can prevent bones along the spine from forming properly, too.
In babies with spina bifida, part of the spinal column often bulges out on the back. The spinal cord and nerves also may be damaged. This can cause problems with movement, sensation and other body functions.
Are there are different types of spina bifida?
Yes, there are three major types of spina bifida:
-
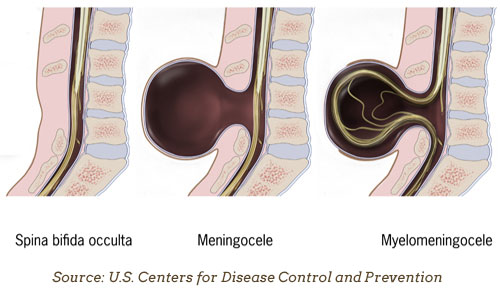
Myelomeningocele: This is the most common and severe type of spina bifida. Babies with this type have part of the spinal cord sticking out of the back.
(See "From Surviving to Thriving With Spina Bifida," below.)
Meningocele: In this type of spina bifida, a fluid-filled sack containing the structures that surround the spinal cord sticks out of the baby's back. The sack is sometimes covered by skin. In most cases, the spinal cord and nerves are normal or only mildly affected.
Occulta: This is sometimes called "hidden spina bifida." There is no opening in the back. The spinal cord and nerves are usually normal and there is only a small abnormality in the bones of the spine. Some people may never have problems from spina bifida occulta and may not realize they have it. Some people will have a small patch of hair on the lower back. However, in some people, the condition can cause back pain, leg weakness or bowel and bladder problems.
What causes spina bifida?
As with other types of
neural tube defects (NTDs), doctors don't yet understand all of the causes of spina bifida. Both genetics and the environment likely play a role. Here's what else we know:
Parents of a child with spina bifida are at an increased risk of having a second child with a NTD.
Certain medical conditions in pregnant women, like diabetes, are associated with increased risk of having babies born with NTDs. Some medications also increase the risk of NTDs when taken during pregnancy.
Folic acid, a B vitamin, can help prevent NTDs when taken before and during pregnancy.
Spina bifida occurs during the first few weeks of pregnancy, often before the parent knows they are pregnant. That's why the American Academy of Pediatrics (AAP) supports the public health recommendation that all women who are able to become pregnant take 400 micrograms (mcg) per day of
folic acid.
How do I know if my child has spina bifida?
Spina bifida may be diagnosed during pregnancy or after birth:
During pregnancy,
several screening tests are done at regular prenatal visits that may identify a baby with spina bifida. These include a blood test, ultrasound and sometimes, amniocentesis, which tests the fluid that surrounds and protects a baby during pregnancy.
After birth, a newborn may be diagnosed with spina bifida when a doctor observes an abnormality somewhere along the spine. An ultrasound, x-ray, MRI (magnetic resonance imaging) or CT (computed tomography) scan may be used to get a clearer picture of the suspicious area.
Are there treatments available for spina bifida?
Yes, treatments are available for spina bifida both before and after the baby is born.
During pregnancy, prior to the birth of the baby: If spina bifida is identified during pregnancy, surgery on the baby may be performed in some patients. Many factors need to be considered when deciding whether or not a pregnant mother and baby should undergo this procedure. If eligible, the surgery should be done at a specialized hospital center experienced in fetal surgery.
After birth: For babies born with myelomingocele, surgery to close the back is usually recommended within the first two days of life. This surgery is necessary to prevent dangerous infections. However, the surgery does not reverse damage that may have already occurred to nerves of the spinal cord. Before and after surgery, babies with spina bifida are frequently cared for in the neonatal intensive care unit (NICU).
In addition to the care provided by a pediatrician, treatments for spina bifida requires a team of specialists. Team members may include neurosurgeons, orthopedic surgeons, urologists, rehabilitation experts, pediatric neurologists, developmental pediatricians, physical therapists, psychologists and social workers.
What other challenges can people with spina bifida have?
Paralysis (the loss of the ability to move). Because nerves leading to the lower part of the body can be damaged in children with spina bifida, the muscles in the legs may be very weak or paralyzed. Joints can also be very stiff. Many babies with this disorder are born with problems in the hips, knees and feet.
Surgery can help correct some of these problems. In addition, muscle weakness can be treated with physical therapy and special equipment such as braces and walkers. Many children with spina bifida eventually can stand and some can walk. The learning process is often long and challenging.
Hydrocephalus ("water on the brain"). Many children with spina bifida eventually develop this condition, caused by excess fluid around the brain. It occurs because the path where fluid usually flows is blocked in spina bifida. The higher up the abnormality is on the spine, the greater the risk is for hydrocephalus. This condition is serious and can be fatal.
Pediatricians may suspect hydrocephalus if the baby's head is growing faster than expected. The condition is confirmed by a CT scan or MRI. It is often treated with surgery to place shunt that drains excess fluid.
Chiari malformation. In addition, most children with spina bifida have crowding of parts of their brain into the spinal canal. This malformation is referred to as Chiari malformation. It's frequently diagnosed by CT scan or MRI. Some patients with Chiari malformation require surgery to take pressure off of the brain tissue.
Urinary tract & bowel problems. Damage to the nerves that control the bladder are more likely to develop
urinary tract infections, which can damage the kidneys. Bowel control may also be a problem. Many medications or procedures can be used to treat these problems in people with spina bifida.
Infections. Children with spina bifida who also have hydrocephalus or urinary tract problems may be vulnerable to infection. Parents of children with these conditions need to watch carefully for signs of infection. Fortunately, the types of infections that can develop with these conditions usually can be treated effectively with antibiotics.
Orthopedic problems. Some orthopedic issues may be noted at birth but others may develop over time. Hip dislocation and scoliosis are common in children with spina bifida. Pediatricians, physical therapists and orthopedists work together to monitor for and treat these conditions and promote motor function.
Latex allergy. People with spina bifida have an increased risk of developing an allergy to latex. It is not known why. To help reduce a child's overall exposure to latex, parents can try to limit their baby's contact with products that contain latex (pacifiers, teething toys, changing pads, mattress covers, bandages and some diapers).
Learning & social challenges. Many children with spina bifida do well in school, although they may be more likely to have
developmental and
learning disabilities that can benefit from
special education. Many also need psychological counseling and
emotional support to cope with their health, learning, and social challenges. Children with mobility problems may need support services through the school system, as well.
Other concerns. Some children with spina bifida may have problems with their
vision. Some may also have problems with sensation. In addition, about 10% to 15% of children with spina bifida also have
seizure disorders (epilepsy). Sleep disordered breathing problems such as sleep apnea are also common.

From Surviving to Thriving With Spina Bifida
By: Melanie Dragovits
 October 25 is World Spina Bifida Day. It is also the day that 18 years ago, I gave birth to our daughter, Elizabeth. Lizzy happens to have spina bifida. She was born with a
myelomeningocele near the two bottom vertebrae of her spine.
October 25 is World Spina Bifida Day. It is also the day that 18 years ago, I gave birth to our daughter, Elizabeth. Lizzy happens to have spina bifida. She was born with a
myelomeningocele near the two bottom vertebrae of her spine.
The exposed spinal cord tissue on her lower back back was flat, covered with a thin membrane and shaped like a butterfly. Her very first surgery to close the open area of her spine happened immediately after delivery. It would be the first of many.
Lizzy was also born with hydrocephalus and needed shunt surgery to drain excess fluid around her brain. In addition,
Chiari malformation was causing crowding of her brain stem. Our rosy-cheeked baby soon looked pale and needed ventilator support and tube feeding. She underwent a very delicate and risky surgery to decompress the back of her brain and brain stem, intended to revive her drive to breathe and other vital life functions.
Lizzy was able to come off the ventilator. However, she still needed a tracheostomy, a surgically created hole in her windpipe, to treat her narrow airway and sleep apnea. Once Lizzy was able to come home, we enlisted a team of home physical therapists, occupational therapists and speech therapists. They were miracle workers. The baby we were warned may not live and, if she did, would not walk, talk, or eat, was eventually doing all of those things!
 Lizzy has grown into a spunky, happy, wonderful young woman adored by many. Throughout her school years she has tried and conquered many goals: swimming, cheerleading, dancing, horseback riding, public speaking, volunteering, getting straight A's, being an active member and leader of high school clubs, acting in a play, learning to drive and more.
Lizzy has grown into a spunky, happy, wonderful young woman adored by many. Throughout her school years she has tried and conquered many goals: swimming, cheerleading, dancing, horseback riding, public speaking, volunteering, getting straight A's, being an active member and leader of high school clubs, acting in a play, learning to drive and more.
One of her most prized accomplishments has been becoming a counselor-in-training for her beloved
Camp Independence. She loves it because she gets to work with younger children who have spina bifida.
Today, Lizzy is a senior in high school with aspirations to be an early childhood educator specializing in special education. Before leaving for college, she plans to attend a
transition program offered by our state. It helps teens with physical disabilities develop skills they need to transition to independent living.
Yes, Lizzy had a rocky and complex start to life. All that has happened shaped her into who she is today, and who I am. The experiences we shared on her journey with spina bifida has enriched our family in countless ways. We look forward to continuing to help others on their own personal spina bifida journey.
Melanie Dragovits is a mother of three and an advocate for individuals with spina bifida. She is also an educator working in the field of special education. She sits on the Family Advisory Board for Ann and Robert H. Lurie Children's Hospital's Spina Bifida Clinic in Chicago.
Remember
Good medical care can greatly improve the quality of life for children with spina bifida and help them reach their full potential.
More Information
About Dr. Gordon-Lipkin
 Dr. Eliza Gordon-Lipkin, MD, FAAP, a candidate member of the American Academy of Pediatrics (AAP) Section on Neurology, is a child neurologist at the National Human Genome Research Institute within the National Institute of Health in Bethesda, Maryland. She has special expertise in neurodevelopmental disabilities and sees patients with a broad spectrum of genetic and developmental disorders.
Dr. Eliza Gordon-Lipkin, MD, FAAP, a candidate member of the American Academy of Pediatrics (AAP) Section on Neurology, is a child neurologist at the National Human Genome Research Institute within the National Institute of Health in Bethesda, Maryland. She has special expertise in neurodevelopmental disabilities and sees patients with a broad spectrum of genetic and developmental disorders.
|
About Dr. Lipkin
 Paul Lipkin, MD, FAAP, is a Professor of Pediatrics at the
Kennedy Krieger Institute and the Johns Hopkins School of Medicine, specializing in Neurodevelopmental Disabilities and Developmental and Behavioral Pediatrics. He has led important national initiatives for the AAP regarding developmental and autism screening and the care of children with neurodevelopmental disabilities. He has been honored as the recipient of the AAP's Arnold J. Capute Award in 2011 for his efforts on behalf of children with disabilities.
Paul Lipkin, MD, FAAP, is a Professor of Pediatrics at the
Kennedy Krieger Institute and the Johns Hopkins School of Medicine, specializing in Neurodevelopmental Disabilities and Developmental and Behavioral Pediatrics. He has led important national initiatives for the AAP regarding developmental and autism screening and the care of children with neurodevelopmental disabilities. He has been honored as the recipient of the AAP's Arnold J. Capute Award in 2011 for his efforts on behalf of children with disabilities.
|