One in every 700 babies is born with a cleft lip, a cleft palate, or both—making it one of the most common birth defects.
Babies born with a cleft lip and/or palate need special care from a team of different health professionals. Their care must be well managed because of the difficult medical, surgical, dental and social factors important to treatment decisions. To help pediatricians better manage children with cleft lip/palate, the American Academy of Pediatrics (AAP) published the clinical report, "The Primary Care Pediatrician and the Care of Children with Cleft Lift and/or Cleft Palate."
The following information explains these recommendations to parents and families involved in caring for a baby born with a cleft lip and/or palate.
Different types of cleft lip and/or palate
The type of cleft lip and/or palate a child has will determine the kind of care that he or she needs.
A
cleft lip means that there is a gap in the baby's lip. The cleft may be on one or both sides of the upper lip and may reach all the way to the nose. Often, a baby with a cleft lip may have a gap in the upper gum.
A
cleft palate has a gap in the roof of the mouth that connects to the nose.
The
combination of a cleft lip with a cleft palate is more common than just a cleft lip or just a cleft palate.
Detecting cleft lip and/or palate
Many, but not all, parents know in advance that their newborn infant will have a cleft lip from the
prenatal ultrasound. The mother's doctor or the baby's future doctor can help parents meet with experts—called a cleft/craniofacial team. Prenatal consultation involves parents meeting various members of the cleft/craniofacial team and learning about the care of children born with cleft lip.
Normally, a cleft palate is not seen until after a baby has been born. A nurse, a doctor, or a parent may notice that the top of the mouth looks different. The cleft palate may involve most or just the farthest part of the roof of the mouth.
Common concerns from parents about cleft palates
Being the parent of a newborn with a cleft lip, cleft palate, or both can feel overwhelming. Simple things like feeding your baby might now be more complicated. Parents wonder how people may react when they see their baby has a cleft lip. Parents also worry how the cleft lip or cleft palate will affect their child long-term—socially and developmentally.
If you are worrying about any of these things or others, talk with your child's pediatrician. They can help answer questions and even direct you to a parent support group near you.
Feeding a baby with cleft lip and/or palate
In general, babies with a cleft palate either as cleft lip with cleft palate or cleft palate alone, suck weakly and need a special bottle to feed. Support from a feeding therapist, certified lactation consultant, and/or nurse experienced in feeding children with cleft palate is recommended for parents.
A baby born with a cleft lip without cleft palate may also need extra help with feeding. However, most babies with cleft lip can feed from the breast or a normal bottle. This is also true for babies with cleft lip and cleft gum.
Care & treatment from the cleft/craniofacial team
Various specialists will care for your child at different times and stages. The cleft/craniofacial team usually includes nurses, social workers, nutritionists, audiologists, speech-language pathologists,
geneticists, pediatricians,
dentists, orthodontists and pediatric surgeons (otolaryngologists, oral and maxillofacial surgeons, and
plastic surgeons). These providers understand common concerns and know the answers to parents' questions.
First appointment: A newborn should see their cleft/craniofacial team within one week (or as soon as possible) from the day they first leave the hospital. In the beginning, the team will make sure the baby is feeding and growing well. The team will also check for other medical problems common in babies with a cleft lip or palate, answer parents' questions, and discuss the next steps for treatment.
Surgery: Surgical repair of a child's cleft is one part of the care that the cleft/craniofacial team provides.
When will my child need surgery for their cleft?
The most common question parents have is,
"When will my child have surgery to repair his or her cleft lip or cleft palate?" The AAP recommends initial reconstructive surgeries for cleft lip or cleft palate occur within the first year of life.
Cleft lip repair: A cleft lip usually is repaired between 3 and 6 months of age. Many things will determine the right time for surgery; the right time for one child may not be good for another.
Cleft palate repair: A cleft palate is commonly fixed between 9 and 14 months of age. If there is a separation in the gum line, it usually is repaired when a child is 8-10 years of age. A child's cleft/craniofacial team will determine the best time for cleft palate surgery.
Every child is different: Children with cleft lip and/or cleft palate often need additional surgeries and treatments as they grow. For example, they may need braces during childhood. Each child will need different numbers and types of surgeries—why individualized coordination of care is so important. Most children born with clefts will need regular visits to their cleft/craniofacial team until they are adults.
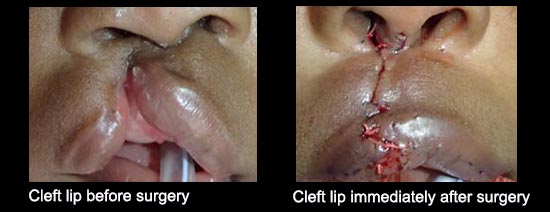
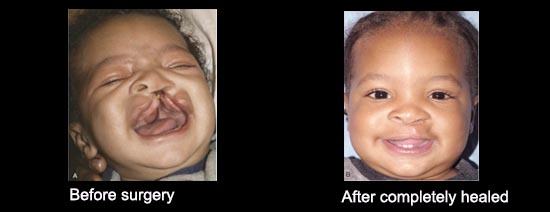
What does a cleft look like before and after surgery?
It is common for parents to worry about how their child will look before and after the cleft lip and/or palate repair.
More information