Photos
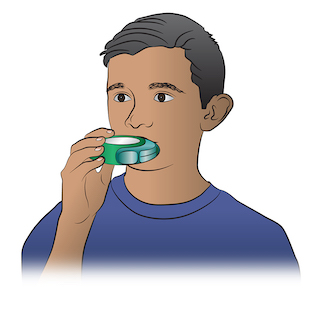
How to Use a Dry Powder Inhaler
Dry powder inhalers require a different inhaling technique than regular metered dose inhalers (MDI). To use a dry powder inhaler, it is important to close your mouth tightly around the mouthpiece of the inhaler and to inhale rapidly. Here are the steps:
- STEP 1 - Remove the cap and follow package instructions to load a dose of medicine.
- STEP 2 - Breathe out completely.
- STEP 3 - Put the mouthpiece of the inhaler in the mouth.
- STEP 4 - Breathe in quickly and deeply.
- STEP 5 - Hold your breath for ten seconds to allow the medicine to reach deeply into your lungs.
- If your doctor has prescribed two or more inhalations, wait 1 minute and then repeat steps 2-5.
Source: Self Care Decisions LLC
Used with Permission from Schmitt Pediatric Guidelines LLC. Text reproduced from the National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma.
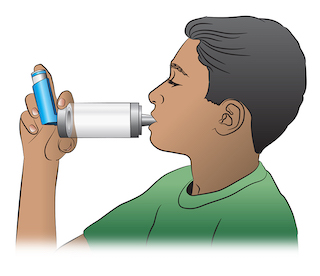
How to Use a MDI with Spacer
A spacer (or holding chamber) can be useful for all people with asthma. A spacer makes it easier to correctly inhale the asthma medicine from the metered dose inhaler (MDI). A spacer is very useful in younger children and older adults.
- STEP 1 - Shake the inhaler and then attach it to the spacer (holding chamber).
- STEP 2 - Breathe out completely.
- STEP 3 - Place the mouthpiece of the spacer in your mouth.
- STEP 4 - Press down on the inhaler. This will put one puff of the medicine in the holding chamber or spacer.
- STEP 5 - Breathe in slowly for 5 seconds.
- STEP 6 - Hold your breath for 10 seconds and then exhale.
- If your doctor has prescribed two or more puffs, wait 1 minute between each puff and then repeat steps 1-6.
Source: Self Care Decisions LLC
Used with Permission from Schmitt Pediatric Guidelines LLC. Text reproduced from the National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma.
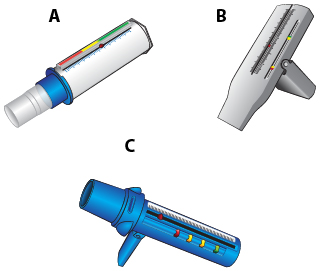
How to Use a Peak Flow Meter
Every adult with asthma should have a peak flow meter. A peak flow meter measures how well air moves out of your lungs. The number that is obtained is called the peak expiratory flow rate (PEFR). The "personal best" value is the highest PEFR number that a person obtains when they are feeling well.
Here is how to use a peak flow meter:
- STEP 1 - Move the indicator to the bottom of the numbered scale. Stand up.
- STEP 2 - Take a deep breath, filling your lungs completely.
- STEP 3 - Place the mouthpiece in your mouth and close your lips around it. Do not put your tongue inside the hole.
- STEP 4 - Blow out as hard and fast as you can.
- STEP 5 - Repeat the process two more times.
- STEP 6 - Write down the highest of the three numbers.
Using a Peak Flow Meter to Determine the Severity of an Asthma Attack:
- GREEN Zone - MILD Attack: PEFR 80-100% of personal best
- YELLOW Zone - MODERATE Attack: PEFR 50-80%
- RED Zone - SEVERE Attack: PEFR less than 50%
Source: US NHLBI
This work is in the public domain because it is a work of the United States federal government. Images reproduced from the National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma.
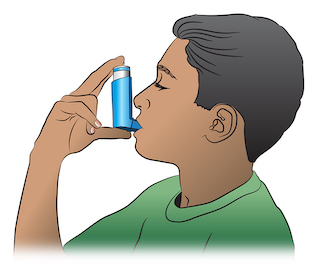
How to Use a Metered Dose Inhaler
A metered dose inhaler (MDI) is a device used to deliver asthma medicine into the lungs. To be sure to deliver the medicine effectively, use the following steps:
- STEP 1 - Remove the cap and shake the inhaler.
- STEP 2 - Hold the inhaler about 1-2 inches in front of the mouth. Breathe out - completely.
- STEP 3 - Press down on the inhaler to release the medicine as you start to breathe in slowly.
- STEP 4 - Breathe in slowly for three to five seconds.
- STEP 5 - Hold your breath for ten seconds to allow the medicine to reach deeply into your lungs.
- If your doctor has prescribed two puffs, wait 1 minute and then repeat steps 2-5.
Source: Self Care Decisions LLC
Used with Permission from Schmitt Pediatric Guidelines LLC. Text reproduced from the National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma.